Background :
The 5-year overall survival rate (OS) for children with thalassemia major who undergo allogeneic stem cell transplantation is 90% and the event-free survival (EFS) rate is 86%. Due to the limited availability of matched sibling donors, the proportion of transplantations from alternative donors is increasing, particularly from haplo-identical donors. Post-transplant infections and graft-versus-host disease (GVHD) remain the major causes of mortality, especially in those who receive transplantation from alternative donors. Post-transplant cyclophosphamide (PTCY) has shown outstanding results of GVHD prophylaxis in haploidentical matched related donors transplantation with hematological malignancies. However, there is insufficient clinical evidence for its application in pediatric patients who received transplantation from haplo-identical donors with non-malignant hematological disease. Here, we retrospectively analyzed the results of 40 cases that underwent allogeneic stem cell transplantation from haploidentical matched related donors (Haplo-RD) and unrelated donors (UD) to evaluate the safety and efficacy of the novel regimen in GVHD prophylaxis.
Method
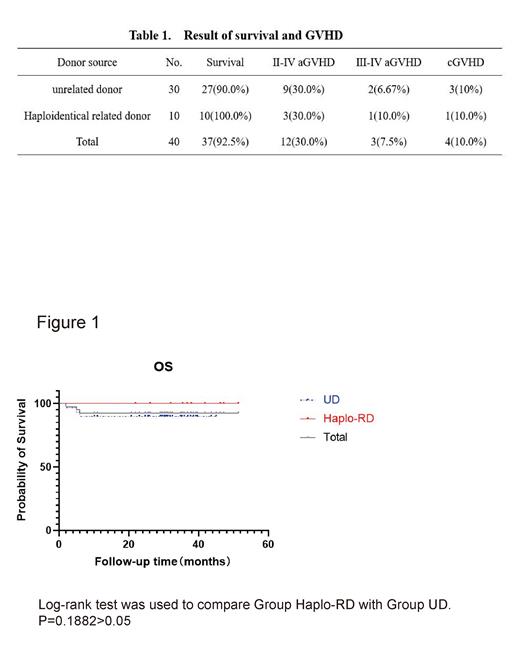
A total of 40 patients with β-thalassemia major received stem cell transplantation, 10 haploid donors (Group Haplo-RD), and 30 unrelated donors (Group UD). Among Group UD, 15 donors were 1 or 2 HLA locus mismatched, remaining 15 were identically matched. The median age of the patients was 5.5 years, ranging from 2 to 12. The Conditioning regimen mainly consisted of fludarabine, busulfan, cyclophosphamide, and thiotepa. GVHD prophylaxis included ATG 1.5mg/kg×3d, cyclophosphamide (CTX) 25mg/kg×2d, cyclosporin A (CsA), and mycophenolate mofetil (MMF). We analyzed the engraftment rate, GVHD incidence, survival rate, and virus reactivation rate for each group.
Results
Engraftment rate was 100%, with a median time of 11 (10-15) days for neutrophil implantation and 12 (6-31) days for platelet implantation. All patients achieved complete chimerism on day 30 after transplantation. Three cases (7.5%) suffered from Ⅲ-Ⅳ aGVHD, with one being in the Group Haplo-RD group and two in the Group UD. Four cases (10.0%) of cGVHD were recorded. The overall survival (OS) rate and thalassemia-free survival rate were both 92.5%. In Group Haplo-RD, both the OS and thalassemia-free survival rates were 100%. Eight cases reported cytomegaloviremia but no one developed to CMV disease. The total activation rate for CMV was 20%. Nine cases suffered from BK virus urinary tract infection, resulting in a total activation rate of 22.5%. Detailed results are shown in Table 1 and Figure 1.
Discussion
Due to the high risk of GVHD and infection, stem cell transplantation from haploidentical and unrelated donors cannot be routine therapy for children with thalassemia major. Standard-dose PTCY regimen significantly increases the risk of CMV and BK infection after transplantation and is not suitable for non-malignant disease. The results have been reported that low-dose PTCY/ ATG can reduce the risk of GVHD as compared with standard-dose ATG in haploidentical donor stem cell transplantation. In our study, the novel GVHD prophylaxis regimen, semi-dose PTCY (25mg/kg×2d) combined with low-dose ATG (1.5mg/kg×3d), was used for stem cell transplantation from haploidentical and unrelated mismatched donors. The incidence of III-IV aGVHD was 7.5% and cGVHD was 10.0%, and there was no rejection of the transplant. The activation rate of CMV and BKV was significantly lower than reported in the literature, and the non-relapse mortality (NRM) after transplantation was significantly reduced. There was no statistical difference in the rate of OS, EFS, aGVHD, and cGVHD between Group Haplo-RD and Group UD. The results provide an effective approach for preventing GVHD and infectious diseases in thalassemia patients who underwent allo-HSCT with high-risk GVHD.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal